Story Highlights
- Obesity linked to diabetes across all age groups
- Among obese adults, increased risk of diabetes highest from ages 35 to 39
- Obesity elevates diabetes risk more for women than for men
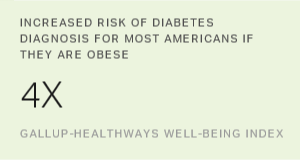
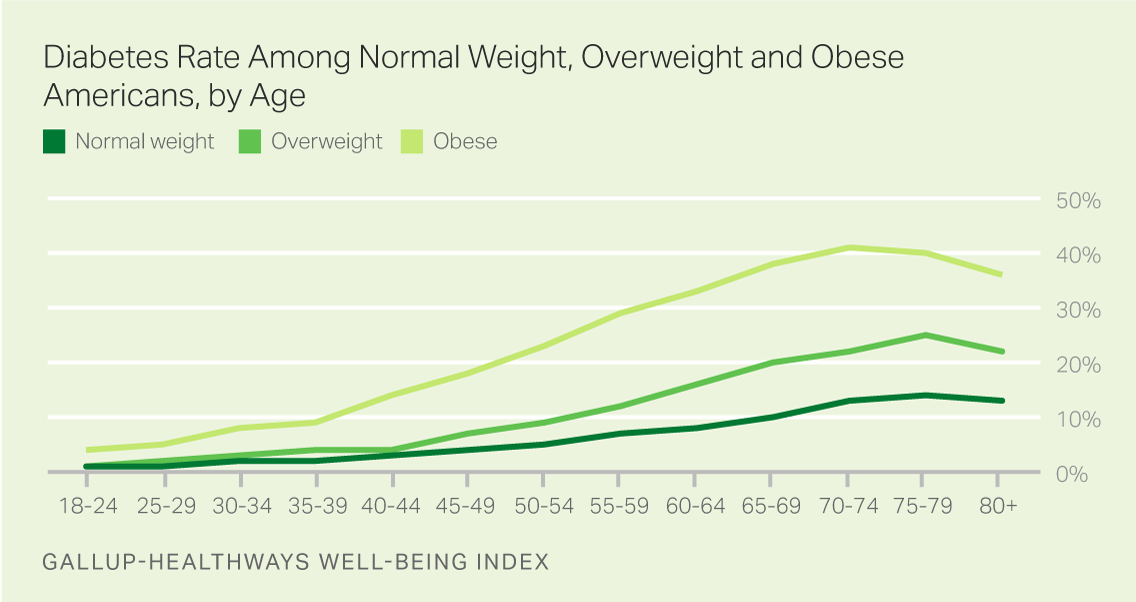
WASHINGTON, D.C. -- Obese adults between the ages of 25 and 64 are at least four times more likely to have been diagnosed with diabetes than those who are normal weight, according to the Gallup-Healthways Well-Being Index. By their mid-to-late 30s, 9.3% of adults who are obese have been diagnosed with diabetes, compared with 1.8% among those who are normal weight.
These results are based on nearly 500,000 interviews conducted in the U.S. from 2014 through 2016 as part of the Gallup-Healthways Well-Being Index.
Unlike some government estimates of obesity, the Gallup-Healthways Well-Being Index uses respondents' self-reported height and weight to calculate body mass index (BMI) and subsequent weight classes. It does not involve clinical measurements that typically result in higher obesity estimates. A BMI of 30 or higher results in an obese classification. Additionally, the Well-Being Index does not discern between Type 1 and Type 2 diabetes, but rather asks: "Has a doctor or nurse ever told you that you have diabetes?"
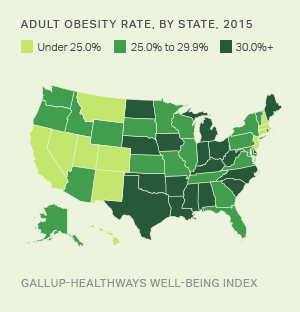
In 2016, 28.4% of all U.S. adults were classified as obese, and 11.6% reported having been diagnosed with diabetes. Researchers from the Centers for Disease Control and Prevention (CDC) have estimated that about Americans born in the year 2000 will be diagnosed with diabetes in their lifetime, and that the percentage of Americans with the disease will from current levels by the year 2050.
Not all individuals who are obese will develop diabetes, and some who are normal weight will get the disease. Factors other than obesity status or age could increase the risk of developing diabetes, including physical inactivity, race and ethnicity, and genetic predisposition.
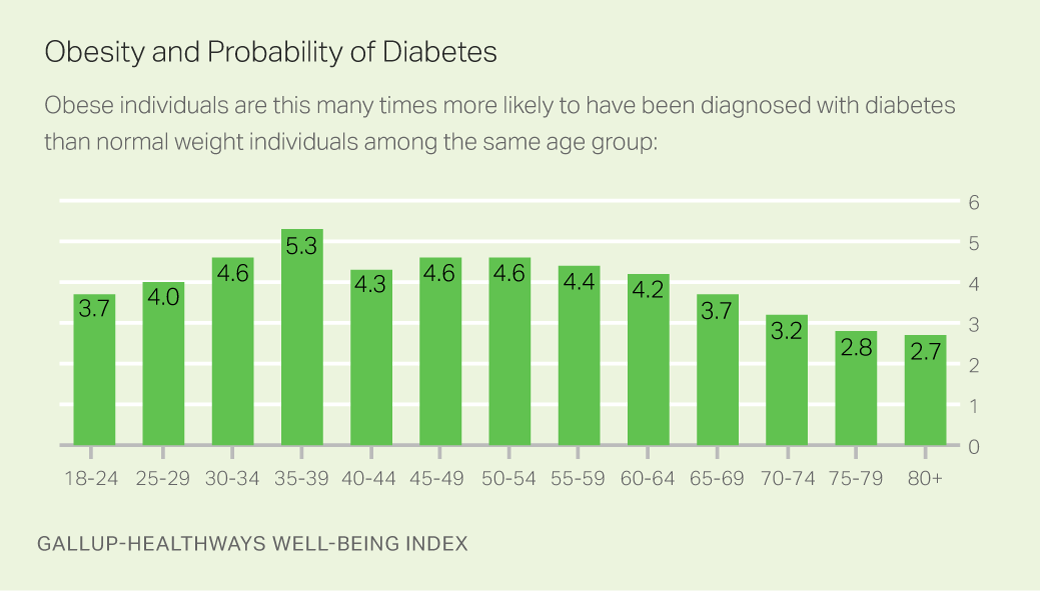
Still, the odds of having been diagnosed with diabetes are substantially higher among those who are obese than among those who are overweight or normal weight, and remain elevated between the ages of 25 and 64. The peak years of elevated risk are between ages 35 and 39. At this stage in life, obese individuals are over five times more likely than their normal weight counterparts to have been diagnosed with diabetes.
Women Have Higher Diabetes Risk Because of Obesity
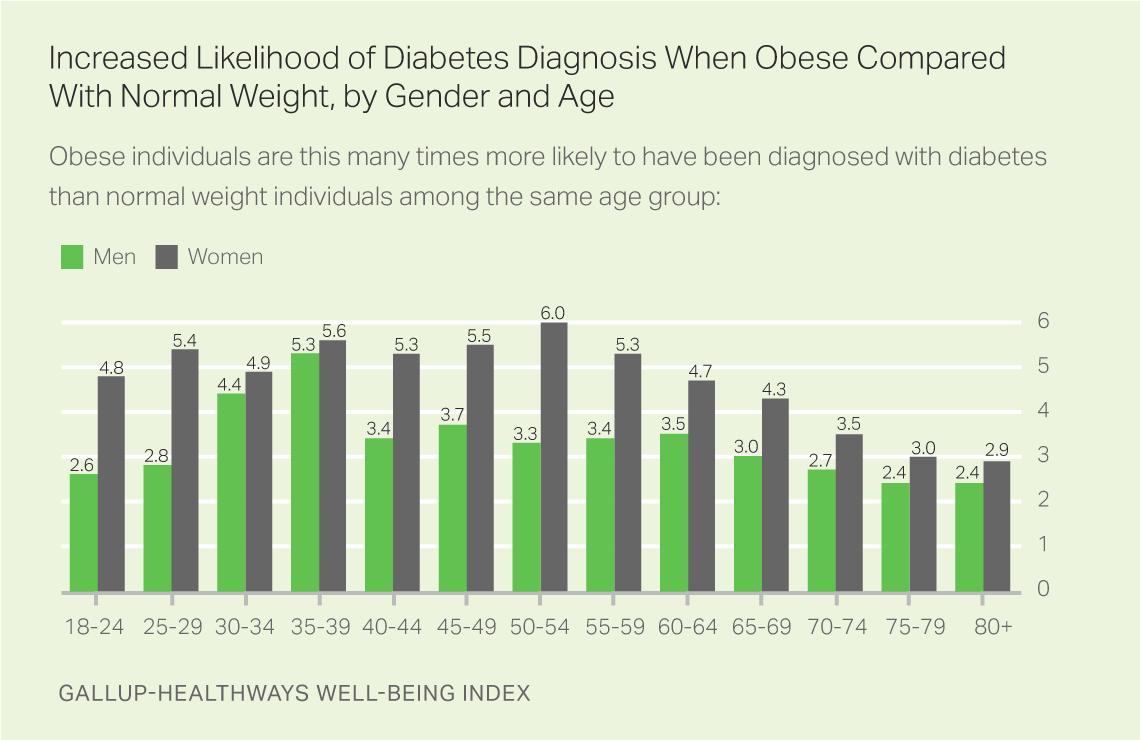
In 2016, women were only slightly more likely than men to report having been diagnosed with diabetes -- 11.7% to 11.4%, respectively. Women who are obese, however, are more likely than obese men to have diabetes across all age groups up to age 60, at which point both groups converge.
The increased diabetes risk is considerably higher for obese women than for obese men across most age groups. For example, obese women aged 50 to 54 are six times more likely than women who are normal weight to have diabetes, while obese men of the same age are only about three times more likely than their normal weight counterparts to have diabetes.
The results of this analysis cannot establish a causal relationship between obesity and diabetes, as individuals are not asked to confirm the age at which they were diagnosed with diabetes and their height and weight at the time of the diagnosis. Some who were obese when interviewed may have been normal weight at an earlier age when they were diagnosed with diabetes, and some who were normal weight (or overweight) at the time of the interview may have been obese at the point of their diagnosis.
The results do, however, add to a significant body of research that demonstrates the unambiguous link between the two diseases: Those who are obese carry a significantly higher risk of developing diabetes.
Implications
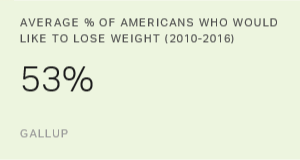
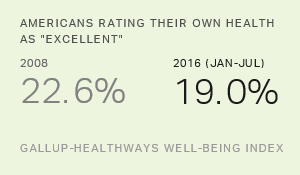
Obesity has in the U.S. since 2008, increasing nearly three percentage points to 28.4% in 2016. This means there are now 7 million more U.S. adults who are obese than would have been the case if the rate had held steady at the 2008 level.
Diabetes, in turn, has climbed by one point since 2008, to 11.6%. Every three-point increase in the U.S. obesity rate is associated with a roughly one-point increase in the diabetes rate.
The findings from this analysis show the strength of the relationship between obesity and diabetes, even for young adults. By their mid-to-late 20s, obese individuals are already four times more likely than their normal weight counterparts to have been diagnosed with diabetes. This increased risk only grows over the next decade before peaking between the ages of 35 and 39. As such, communities, businesses and healthcare providers should pursue efforts to curtail obesity at the earliest possible time and with increased urgency.
The costs of obesity are substantial. In unplanned absenteeism alone, obesity and associated chronic conditions have been estimated to cost the U.S. economy annually. This economic impact is likely exacerbated given that the obesity-diabetes link is greatest among adults in their prime working years.
Curtailing the relentless climb of obesity and associated chronic conditions such as diabetes can be accomplished. Hospitals can put in place diabetes management programs to help people who have already been diagnosed, as well as diabetes prevention programs for those who are at risk.
"The best diabetes management programs are comprehensive -- delivering professional education, inpatient glycemic management, outpatient prevention, and self-management education and support -- and they engage multidisciplinary teams for coordinated care," said Sheila Holcomb, vice president, Sharecare Diabetes Solutions. "They focus on metrics such as achieving glycemic targets and reducing average length of inpatient stays."
Additionally, at the community level, initiatives like the -- an organization that specializes in transforming communities across the U.S. into higher well-being places -- has compiled many success stories.
For example, between 2010 and 2015 the California Beach Cities (Redondo Beach, Manhattan Beach and Hermosa Beach) had a 9.2-point decline in adults who were either overweight or obese, coupled with a 1.1-point decline in diabetes. This was done in part through close planning and cooperation with the Beach Cities Health District to transform both the physical structure of each community and the culture itself, resulting in a population that is healthier and better informed about what is needed to best pursue a life well-lived.
See the Gallup-Healthways report on U.S. diabetes prevalence across states and communities .
These data are available in .
Survey Methods
Results are based on telephone interviews conducted Jan. 2, 2014-Dec. 30, 2016, as part of the Gallup-Healthways Well-Being Index, with a random sample of 484,350 adults aged 18 and older, living in all 50 U.S. states and the District of Columbia. The smallest sample size for all adults is for those who were classified as obese and aged 25 to 29 (n=5,789); the largest sample size is for those classified as normal weight and aged 18 to 24 (n=21,372). These sample sizes were reduced by roughly half when parsed by gender. The margin of sampling error for each reported BMI class within each age group is no more than ±0.2 percentage points in most cases. All reported margins of sampling error include computed design effects for weighting.
Each sample of national adults since Sept. 1, 2015, included a minimum quota of 60% cellphone respondents and 40% landline respondents, with additional minimum quotas by time zone within region. Prior sampling dating back to Jan. 2, 2014, involved a 50% split between cellphone and landline interviews. Landline and cellular telephone numbers are selected using random-digit-dial methods.
Learn more about how the works.