The COVID-19 pandemic has shown us that the perception of risk affects public health policy -- and public behavior -- as much as actual risk.
Results from the Lloyd's Register Foundation , a global survey conducted before the COVID-19 pandemic, show that countries racked by greater levels of worry about being harmed in the course of daily life often went on to adopt stricter COVID-suppression policies and behaviors. Meanwhile, the countries least worried about (pre-COVID) safety and health risks have generally taken fewer precautions, despite being among the most vulnerable to the disease because of high-density cities, thick global travel networks and large elderly populations.
People living in Sweden, for example, express the least concern about mundane risks out of 142 countries and areas surveyed. When it comes to potential harm from food, water, electrical power lines and appliances, almost no Swedes say they are very worried. Violent crime and severe weather register significant concern with 10% and 9% of the population, respectively. By contrast, in Mozambique, 57% of adults say they are very worried about serious harm from the food they eat and 49% about the water they drink. Majorities there are very worried about severe weather (60%) and violent crime (58%), and many worry about serious harm from electrical power lines (38%) and household appliances (34%).
These gaps in concern are evidently grounded in actual experiences. According to the World Risk Poll, those worried about serious harm from a given source are far more likely to report having experienced it or known someone who has. Official records show early death and severe injury are much more common in Mozambique and lower-income countries than in Sweden and higher-income countries, according to data from the .
Experience with risk has shaped the response to COVID-19. Sweden is well-known for initially declining to issue stay-at-home orders or close restaurants and other businesses, require masks, or otherwise issue more than minor restrictions on its population, which has a relatively older and urbanized population. In mostly rural Mozambique, by contrast, the average age is 34 (compared with 48 in Sweden) -- but schools and some workplaces there closed when the pandemic began, and masks are required. The actual threat has been far greater in Sweden. Mozambique has seen only four deaths per 1 million people from COVID-19, compared with 626 per million in Sweden.
The influence of the recent past is apparent in East Asia. In Taiwan, Hong Kong, Japan and South Korea, mask-wearing became even more widespread after the 2003 SARS epidemic -- and they enacted other disease-suppression habits, leaving those countries and areas well-prepared for the current crisis.
This pattern -- where relatively recent past experiences related to either safety or trauma guide present behaviors in addressing the same ostensible situations -- means that high-income countries, especially the United States and many in Europe, have taken fewer precautions than many countries in the developing world. Whether countries overreacted or underreacted will likely be debated for years to come, but it is clear that people living in different countries perceived the risks from COVID quite differently.
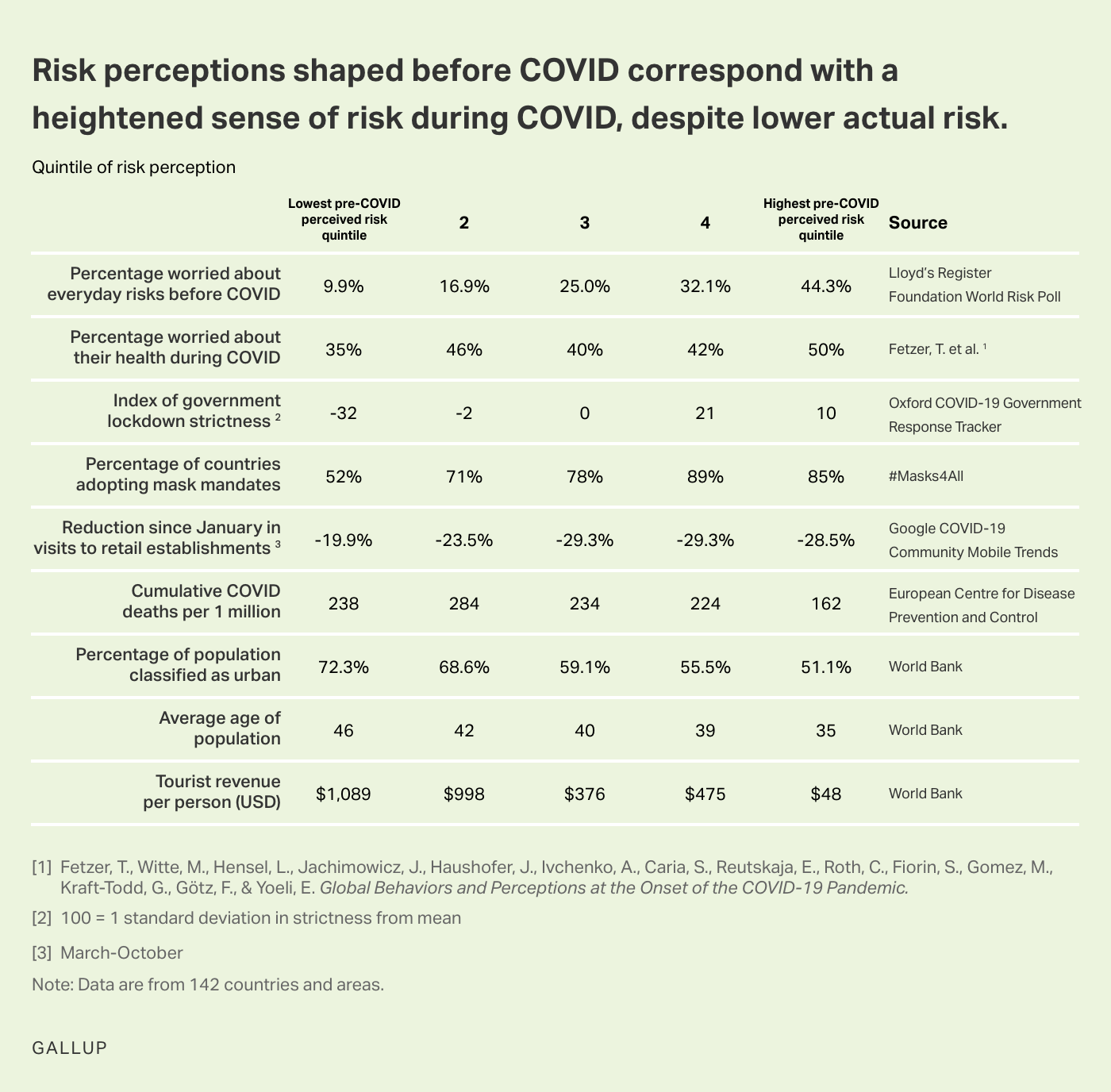
Chart. This chart plots different statistics from a variety of sources, including the percentage of the population worried about everyday risks before the COVID-19 pandemic, the average age of the population, tourist revenue, and countries adopting mask mandates by overall risk perceptions before the pandemic.
The disconnect between perceived risk and actual risk is personal. Results from a survey conducted early in the pandemic by economist Thiemo Fetzer from the University of Warwick and his collaborators showed that older people had similar levels of worry about their health as younger people, despite being at much greater risk of death. People living in countries and regions with relatively high COVID-19 death rates (the United States and Europe) were also less worried about their health at the onset of the pandemic than those living in places with lower death rates, such as Africa and East Asia.
The varying perceptions of risk have motivated varying actions. Those who say they are worried about their health exhibit much more cautious behaviors and endorse stricter rules and enforcement of social distancing, a concept psychologist have deemed "functional fear."
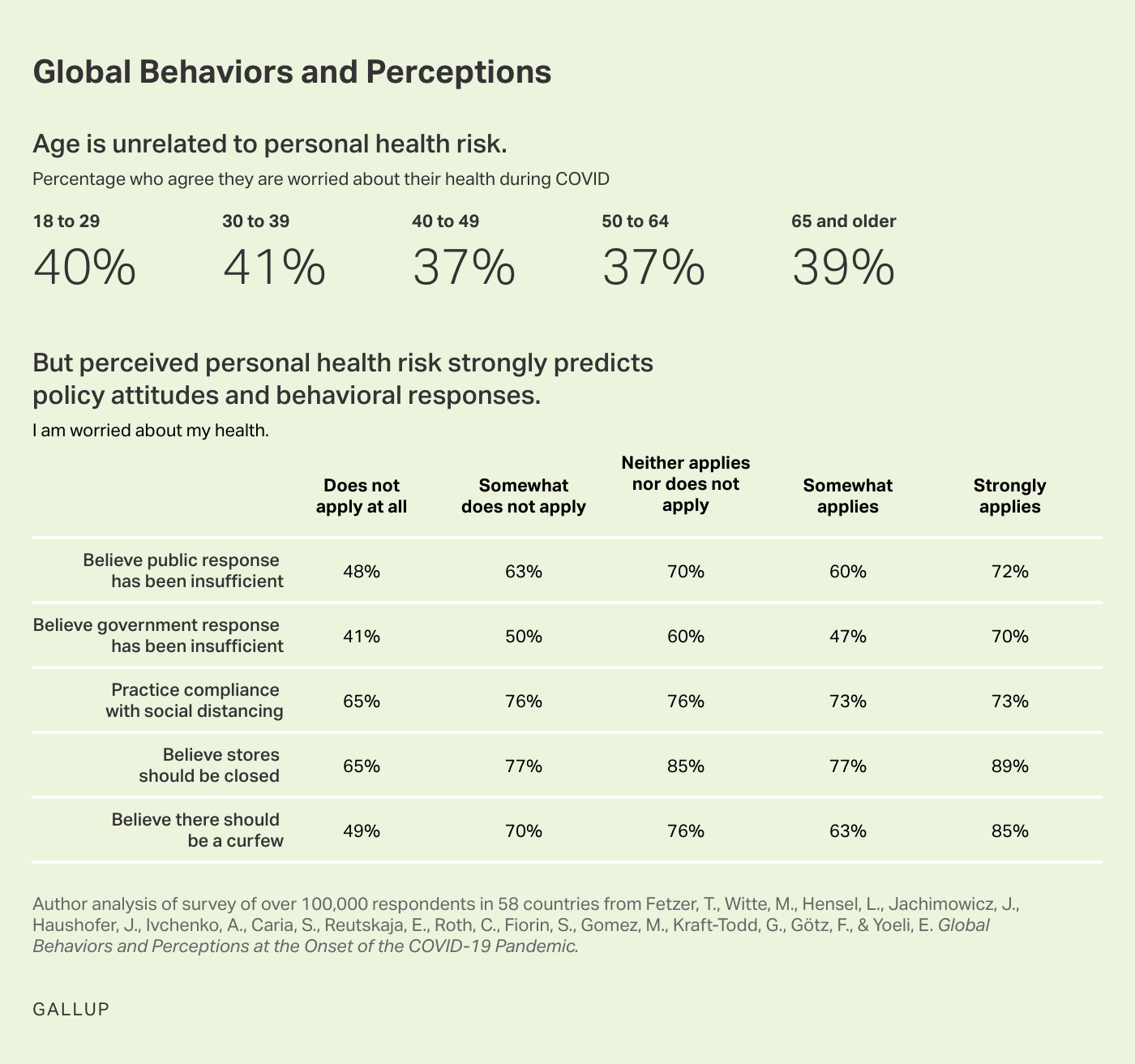
Chart. This chart displays the relationship between age and people's worry about their health during the COVID-19 pandemic, and the relationship between people's worry about their health and attitudes and behaviors in regard to COVID-19 policies.
This connection between fear and policy is playing out right now in the United States, as Gallup's research with Franklin Templeton has shown. Those who express greater fear of the virus are far more likely to favor restrictions on schools and businesses as well as other disease-suppression measures.
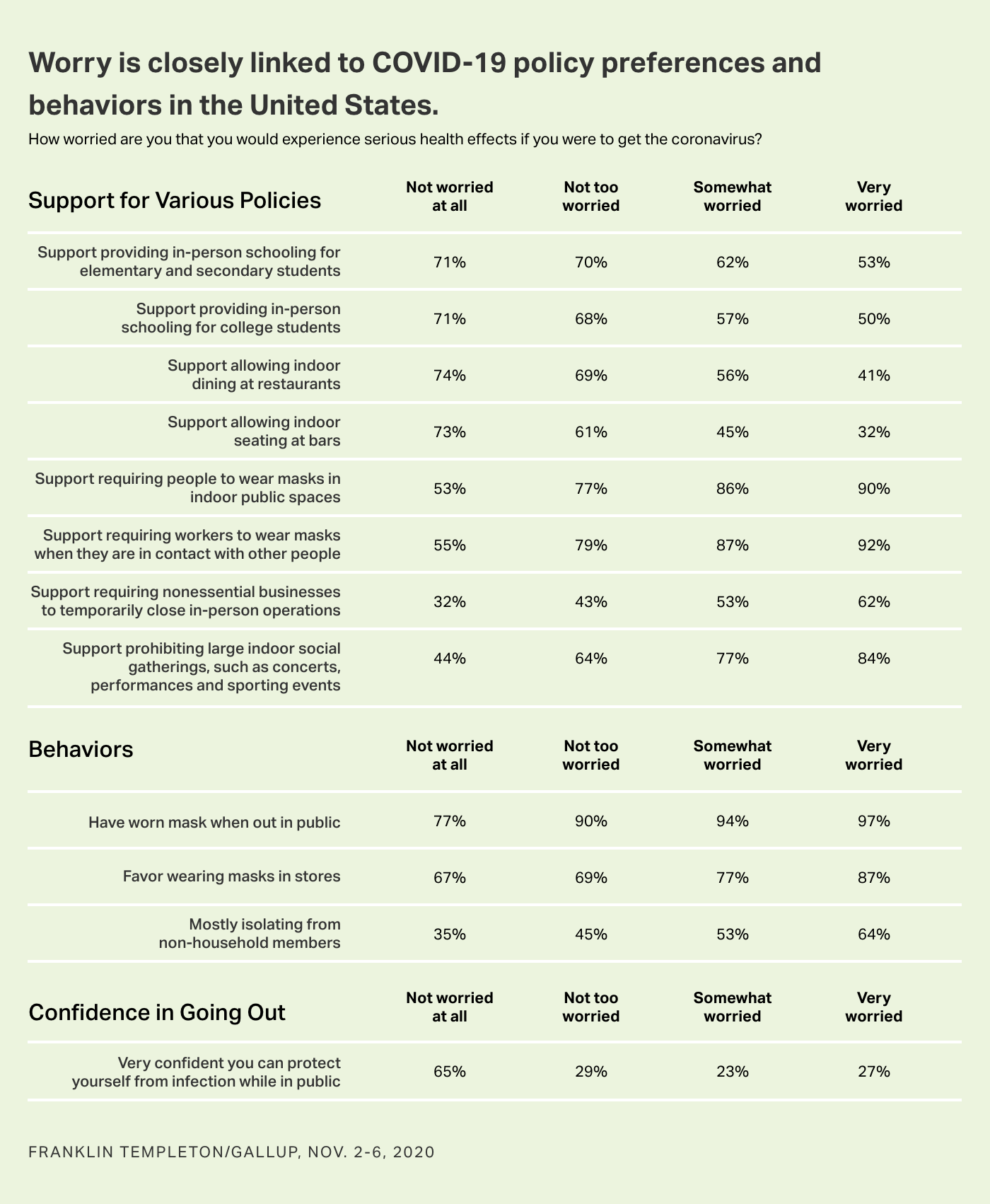
Chart. This chart plots COVID-19 policy preferences, behaviors during the pandemic, and people's confidence in going out by the level of worry people have about experiencing serious health effects if they were to contract the coronavirus.
Moreover, the policy preferences and perceptions of risk have a partisan edge. tend to overstate the risks to young people, and Republicans tend to understate the lethality of the virus more generally.
If President-elect Joe Biden wants more Americans to take greater precautions until they receive a vaccine, he will need to convince many who have not been harmed that the risks are nonetheless serious, either to them or to others. On the other hand, exaggerating the threat from COVID will make it easier to dismiss. In the United States and a number of other prosperous nations, logical conclusions from evidence-based research will have to serve as the impetus for behavioral change, in the absence of a recently shared collective experience of harm.




