Stryker's new system for hip replacement surgery was an important step forward. The technology was unthinkable a generation ago.
Called a "navigation" system, it was designed to use electronic devices anchored to a patient's pelvis and thigh bone combined with sensors locked onto operating instruments to help the surgeon place the new joint in just the right spot. The surgeon could see the positioning of the artificial joint into the hip on a computer screen, thereby eliminating less precise estimations.
 |
Getting the joint perfectly aligned gives a patient much better range of movement when doing something as simple as sitting or walking up stairs. With conventional surgery, the acetabular shell -- the cup into which the ball of the thigh bone fits -- might not be aligned as well, reducing movement and even creating a risk that the hip could dislocate.
Solving this kind of surgical problem was exactly the sort of innovation upon which Stryker is built: a profitable product in high demand, incorporating medical and technological advances that improve the lives of its clients' patients. Hopes and expectations were high.
Soon after field testing began in 2004, Stryker's hip navigation systems were being returned to the company with complaints from orthopedic surgeons, says Dr. Amir Sarvestani, a project manager in the company's research and development facility in Freiburg, Germany. "Just a few days after we shipped the product to customers, unexpected problems were identified," says Sarvestani. "We couldn't believe what we saw when our instrumentation came back."
"Pieces were broken and beaten up, and the electronics were frequently not functioning like they should have been," says engineer Dieter Teschke. "We said, 'What's happened to this instrumentation?'" No one had anticipated what the devices would endure in a hip replacement surgery.
The responsibility for fixing the problem fell to team leader Klaus Welte, vice president and plant manager in Freiburg. His team would need to meticulously rethink each component and strengthen it against the stresses that were being applied through repeated, high-impact use. He also needed to assemble his team in the same way as the product, each employee well-fitted to his role and working flawlessly together with the rest. The failure of any component, or any team member, could cause the product and the entire group to fall short of their goals. By understanding as much about each other as they did about the various components of the new system, Welte's team improved the science of hip replacement.
Customers who are worlds apart
The facility in Freiburg was owned by Leibinger before it was acquired by the Stryker Corporation in 1998. Leibinger specialized in software that used three-dimensional X-ray or magnetic images of a patient's brain. These images helped neurosurgeons plan the operations they needed to perform. After becoming part of Stryker, the Freiburg division extended its work into developing surgical tools guided by the same navigation technology.
 |
"We developed a system that consists of a pointer -- a wand the surgeon holds in his hand -- that he can use during the operation," says Welte. "Through the pointer, we were able to create a link between the actual patient during surgery and the image that was created of the patient beforehand." The pointer and image allow the surgeon to know precisely where he is inside the patient during surgery.
The next logical extension of the Freiburg team's work was into orthopedic surgeries, which make up a much larger part of Stryker's business. Hip and knee replacements are far more common than brain surgery, particularly as advances in healthcare allow more people to live longer. The company figured if the same combination of software, tracking, and imaging could be incorporated into bone operations, it could substantially improve hip and knee surgeries, while creating another source of revenue.
"Stryker believes that our image-guided systems are integral to the future of total joint replacement surgery," the company said in its 2003 annual report. "For this reason, [in addition to a knee navigation system] we are also developing a hip navigation platform that will support less invasive hip replacement with smaller incisions and more accurate placement."
But as the Freiburg engineers were about to find out, instrument design for orthopedic replacements differs from instrument design for neurosurgery in one crucial aspect: sheer force. The brain is composed of soft tissue, and the instruments used for surgery on it are relatively delicate. "Our company came from a history of neurosurgeries," says Teschke. "Before this, we made micro-instrumentation and micro-implants for brain and head surgeries. The difference between those customers and the orthopedic customers? They're worlds apart."
As anyone who has ever seen one can attest, a hip replacement surgery, while at some stages done with a light touch, necessitates a certain amount of bone cutting, grinding, reaming, and pounding on the instrumentation with a hammer. "It looks brutal," says J眉rgen Pross, another member of the Freiburg team. "Actually, it looks like working in a garage, fixing a car."
 |
Further complicating the design specifications, the surgical tools have to be repeatedly sterilized. Between surgeries, they are placed in an autoclave, a sort of medical pressure cooker in which 270-degree-Fahrenheit steam at high pressure kills any bacteria that could endanger the patient. Not only did the metal in the instruments have to maintain its integrity through repeated cycles of being struck and heated, the precision electronics had to continue to function perfectly.
While Stryker had been successfully manufacturing electronics to be "autoclavable" for years, the addition of the impact stress created another level of complexity: The electronics could be affected by the pounding during surgery or the heat of the autoclave. As for which stress was causing the electronic problems, "Actually, that was sometimes not so easy to answer," says Pross. "We didn't know at that time." In addition, the repeated heating and cooling made some of the buttons on the instruments stick or caused the infrared sensors to rise from their flush positions in the metal housing.
"If you look at the situation as a curve, the curve was going down into a deep valley," says Sarvestani. "The trust in the reliability of a new product is of utmost importance to our customers and to our sales force." The issues had to be resolved before going to market.
Three challenges in one
The reputation of the Freiburg group was on the line. Because of the urgency of fixing the problems, a team of Stryker engineers in Kalamazoo, Michigan, was asked to give advice and double-check the design. While the assistance was appreciated, it added to the pressure. "We knew that we had only one chance to fix this problem and that if we would fail, it would have a big impact on the organization here," says Pross.
The challenge for Welte was assembling and directing a team of the right people who could put the hip replacement system back on track. To succeed would require both a clear view of what had to be accomplished and a deep understanding of each team member's abilities.
"We have a very well-defined [product development] process," says Welte. "The key performance targets are defined for the product, and we continually refine them over time. That gives the team a pretty clear direction on where they should be going and what are the right questions to ask." The difficulty was not in understanding what had to be done, but in actually designing a hip replacement system that could simultaneously maintain its electronic circuitry while enduring the mechanical stresses of the operations and the heat and pressure of sterilizations.
"Nobody had ever achieved meeting all these three requirements at the same time," says Sarvestani. "It's very simple to meet one requirement -- for instance, to make it very robust to withstand the impact. The challenge was to look at all the requirements at the same time and to make sure that we had good coverage of all of them."
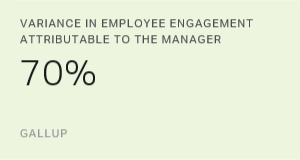
With the high pressure and external stress of finding a solution for the hip navigation system, it was important to get the interpersonal nuances right. In their favor, the employees began with a good understanding of themselves and of each other's talents. "We do one-on-ones with our employees very often -- every two or three months at least," says Welte. "In those, we really ask them, 'What do you do best?' and, 'What do you like about your job?' We try to help people understand themselves. What they describe they do best is really what gets exactly to the role we want them in." In fact, on the third item in Gallup's 12-item employee engagement survey (Q12) -- which states, "At work, I have the opportunity to do what I do best every day" -- the Stryker team ranks in the top 15% of workgroups in Gallup's global engagement database. (See "The Third Element of Great Managing" in the "See Also" area on this page.)
Welte assembled a team of the best people at Freiburg in operations, computer-aided design, engineering, and research. He looked to Sarvestani for "structured analysis," thorough communication, and follow-through. Pross, who had more friends in the building than anyone else on the team, provided the "social glue." That, combined with a high degree of responsibility -- "He would never stop until everything is complete," says Welte -- made him central to keeping the project moving. Teschke is a natural organizer and always well-grounded in the facts. "He takes the speed out if the team gets ahead of itself," says Welte. Operations Manager Michael Porbadnik is particularly talented at understanding how a design will stand up to the manufacturing process.
When the team is designing systems rather than fixing problems, Welte also relies on Jose-Luis Moctezuma. He serves as an in-house visionary whose ideas, such as a gravity sensor in the overhead locator that tracks the position of all the other components, at first seemed unorthodox, but later turned out to be "not only useful, but imperative," says Welte. "And, he knows as much or even more about orthopedic surgery than many orthopedic surgeons." In the natural conflict of perspectives -- Moctezuma eager to jump forward and Teschke cautious to not move too fast -- the team found the optimal path.
 |
Asked about his own greatest talents, Welte says, "I analyze things and see their properties, and I work to put them together in an ideal combination." He enjoys doing this both with the devices Stryker creates and with the members of a team. "If you combine technology, you see a much more rapid result," he says. "With people, it takes longer to see the result."
"A very, very unpleasant room"
Once he had these key players in place, Welte looked for holes in the team's abilities. "After we have a team assembled and the team starts its work, we analyze what they are doing, and we see what's missing," he says. "We are looking for the missing piece of the puzzle. At the same time, I have a mental picture of each person and what he contributes, what he does best. To find that missing piece, we look through our list of people and ask, 'Who is the person that has the best ability to fit into that puzzle and fulfill the specific role that we need at this time?'"
"Creating an effective team requires more than just filling all the job descriptions with someone who has the right talent and experience," says Welte. "By no means can you substitute one engineer for another. There are really very, very specific things that they are good at." And how well the team members' abilities combine is as important as the abilities themselves.
"It usually takes about six months or more to find out exactly about a person," says Welte. "Sometimes it's also quite surprising, because it's not always what you saw in their r茅sum茅. There have been several cases in the past where we hired somebody and then ended up after, let's say a year or so, reassigning him to a totally or a significantly different task."
As an example, Welte mentions an engineer hired as a research and development manager who turned out to be somewhat risk-adverse but intensely drawn to performance metrics. His cautiousness handicapped him at the beginning of projects, when numerous possibilities need to be explored without inhibition, but made him well-suited for the later stages, when it is crucial to make sure everything is right.
The newly formed team took over a meeting room as their central gathering point, where they would spend about half their time together for the next six months. They called it the war room -- "a very, very unpleasant room," Welte recalls. "Everybody felt the situation so intensely that we had the feeling that we were right in the middle of a war fighting against these problems," says Pross.
There were no simple solutions. Each aspect of the instruments had to be analyzed separately, and about 10 problems had to be rectified. "The only way to get out of that situation was to work hard," says Teschke. Examining the broken predecessors, the engineers pinpointed where electronic connections were breaking from the surgeon's blows. They spent three months determining the right glue for capacitors; that had previously been a weak link. A different welding technique was used to encapsulate the electronics within the shaft of the probe. After testing various metals for the buttons, the team found one that would not expand with repeated sessions in the autoclave.
Things started to click. "There was the point where we as a team really started, in a systematic way, to dig down to the problems and work on systematic solutions," says Pross. "That really raised the confidence in everybody that we were [onto a good way] of solving the problems. From every perspective, the knowledge came into play. The test plans got much better than before. The design was really reviewed in each and every aspect. And the more we progressed in a systematic fashion, the more the team was confident that we were close to a solution."
Sarvestani was impressed with how the various talents of the team members combined into an effective and collegial group that made all its major decisions by consensus. "It was true teamwork," he says. "We had some people who were very strong in mechanics, and others who were stronger in electronics, others who were strong in processes, others who were strong in how to validate designs. That was all brought together into one master plan."
Because of the number of problems, the team didn't attempt to solve them simultaneously and assemble the full set of untested solutions in one prototype. Instead, they solved the issues one by one, beginning with the most crucial and working their way down to the relatively minor. This meant the group didn't get to see a fully assembled prototype until they had tackled the full list of solutions.
"The most encouraging situation was when we did the pre-pilot test," says Sarvestani. "We assembled all the components, and for the first time, we could see that the entire design -- after all the changes and improvements we did -- was working."
 |
As the initial introduction made painfully clear, it was one thing to make a working instrument, but quite another to make one that looked and worked the same after many surgeries and sterilizations. To guarantee reliability, the team hired a group of local students and procured a robot (one of Porbadnik's ideas) to put the prototypes through the same conditions as in a hospital. The robot moved instruments into and out of the autoclave around the clock, through 600 heating and cooling cycles. Working in continuous shifts every day of the week, the students loaded freshly autoclaved devices into "impaction machines" that mimicked the pounding they would take in an operating room. "The whole building was shaking," says Teschke.
Even with continuous testing, the redesign of the hip navigation system took four weeks longer than upper management had hoped. But the devices came through with flying colors. The LEDs lit up after autoclaving. None of the buttons or moveable parts stuck after repeated heating and cooling. There were no cracks in the housing after the instruments took a pounding. Through a long list of criteria, the work passed its inspections. "We had 100 percent success -- 100 percent of the instruments passed our test criteria," says Teschke. "From a quality standpoint, this project brought our whole hardware electronic team to another quality standard. It was fantastic what we learned in this short timeframe."
There was no celebration when the improved hip navigation system was shipped to orthopedic surgeons around the world. The team was simply too nervous and didn't want to claim victory until the device proved itself in larger numbers and under actual operating conditions.
The nature of design work is that the number tested is usually far less than the number manufactured. "That makes it very difficult to conclude from your own results how the product will perform later in the field, where the sample size is much bigger," says Sarvestani. "That was one of the reasons why we were always skeptical, even after it passed all the tests and we released it. None of us was really totally convinced." The team waited for news from the field.
"No news is good news"
They have a Bavarian saying about success: "Nicht gescholten ist Lob genug" -- Not being scolded is praise enough. Or, as Americans would say, "No news is good news." In the medical devices industry, when a product has problems, the reports and the devices come back, just like the first version of the hip navigation system did. Success is much quieter. For all the effort they put into creating a system to give surgeons instantaneous, detailed, and accurate feedback, the Freiburg team received silence -- precisely the wonderful, reassuring silence they hoped for.
"We're now one-and-a-half years after we released the instruments," says Sarvestani. "For the first nine months, we didn't have a single complaint. That is an incredibly low number for this type of instrument."
The team's hard work allowed Stryker to make good on its promises to the market -- and to trumpet in the annual report released in spring 2005: "Stryker pioneered the emerging field of image-guided surgical navigation, and we remain the only company to develop fully integrated navigation hardware and software."
Team leader Welte is less effusive than his colleagues, partly by nature. "I'm a person who is never really 100 percent happy with the way things are. I like constant improvement," he explains. Nonetheless, he says he is quite pleased with the way the team meshed, got the product back on track, learned more about each other's talents, and increased their capabilities in the process.
"That was a big victory for us."