Hospitals try to deliver the best health outcomes. That's a given. But many also aim to deliver high levels of customer service. On that latter goal, healthcare systems are falling short. Here's why: Truly improving service demands a culture that intentionally champions a focus on the patient.
Managers must be equipped to drive employee engagement in their departments.
What healthcare systems urgently need are clear intentions and strategies at the leadership level. These will determine whether a service mindset can exist within a hospital. What's more, getting employees engaged and connected to this mission will ultimately determine whether they live out that mindset each day.
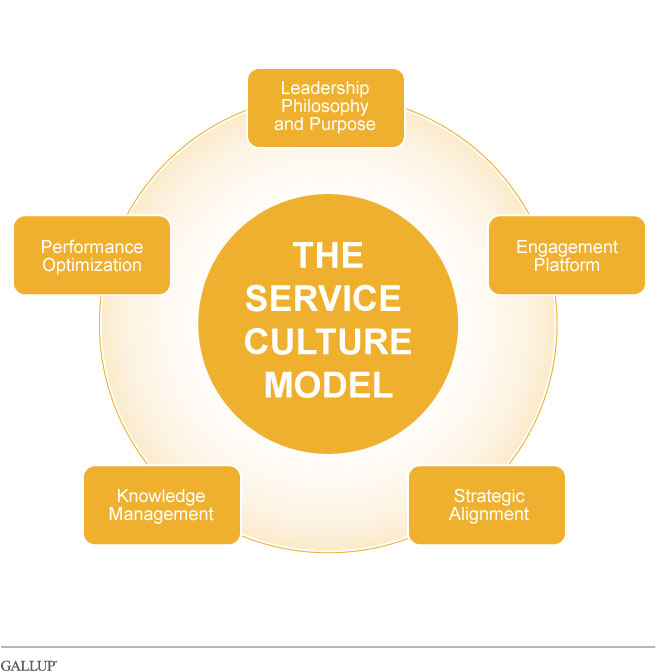
优蜜传媒has found that a service-centered culture requires:
-
a committed leadership team that champions a philosophy that is aligned with service
-
employee commitment to providing outstanding service and quality
-
the strategic alignment of the organization's plan, policies, and procedures with the goal of being service-focused
-
an established process to document and disseminate organizational knowledge and efficiencies
-
an ongoing commitment to improving performance and using proven tactics
It's difficult to execute any vision for change in a service-oriented industry -- even when leaders clearly communicate it to the organization -- without an engaged and motivated workforce. Healthcare systems with a strong service-oriented culture recruit and hire people who fit that culture and begin sharing the vision during the recruitment phase and through orientation and onboarding.
A healthcare system must implement regular feedback mechanisms in the early stages of a healthcare professional's tenure. The organization should check in with new hires after 30, 60, and 90 days, using these opportunities to assess whether the recruit is adapting to and thriving in the organization's culture. The healthcare system should also continue to provide ongoing training and development, giving refresher courses about the vision and culture every 12 to 18 months. With leadership's support, these engaged employees become ambassadors for the patients' priorities.
After proper onboarding, a healthcare system must align its human resources policies to encourage service excellence and hold employees accountable to the standards. Managers must be equipped to drive employee engagement in their departments and held accountable for action planning and knowledge sharing. Aligning these activities with the hospital's larger strategic plan and organization-wide goals is crucial and should be transparent from leadership down to the front line. One of the greatest challenges in any modern and multi-location system is that pockets of excellence exist, but best practices are rarely shared across units. Maintaining open and intentionally structured communication is a means to spread great customer service across an organization.
As in other service-based industries, consistency is key. A patient may interact with many areas of a hospital over the course of an inpatient stay, a series of tests, or a surgery. Receiving fantastic service in one area and mediocre service from another lowers a patient's perception of the overall experience he or she has had.
Finally, every hospital must have a built-in mechanism for improving performance. Building performance improvement teams and using the Plan, Do, Check, Act model can help ensure that performance improvement is an understood and respected part of the culture.
What strong service cultures do right
Improving the patient experience is about changing a hospital's culture.
Healthcare systems that can achieve a patient-focused service culture take improving the patient experience as seriously as improving financial and clinical outcomes. Gallup's studies of healthcare systems that have built a strong service culture yield some dominating themes:
-
Strong and visible leadership that not only is committed to the patient experience but also is able to instill that commitment in the rest of the organization. There are typically two strong leaders involved in the process -- a managing director or CEO who sets the vision and a head of nursing who helps execute the strategy.
-
A clear mission, vision, and values and a set of behavior standards that capture the intent of the organization and create accountability for service among staff members. These are not simply words on a page. Rather, hospitals must reinforce these beliefs and behaviors at orientation, staff meetings, and daily huddles. Ideally, facilities use real patient examples to ensure that the mission, vision, and standards resonate throughout the hospital.
-
Consistency across all messages so that managers and staff see the patient experience as a strategic objective that is as important as other financial and clinical outcomes. It's essential that healthcare systems consistently communicate what constitutes the proper patient experience not only in the strategic plan but also in job descriptions and performance evaluations.
-
Buy-in from key constituencies, including physicians and the broader patient community. Negative relationships with either group can adversely affect a healthcare system's change effort. Physicians are particularly sensitive when they don't feel they have been involved in a significant directional shift. The general public -- which includes past patients and their families as well as potential patients -- also can form perceptions about a healthcare system's brand based on their or others' previous experiences. So hospitals must be deliberate in their messaging to overcome any lingering problems.
-
A family atmosphere that cuts across unit and departmental lines in every hospital. Creating this type of environment starts by recruiting and hiring people who fit the kind of culture that provides the best possible patient experience. Leaders and managers must make a point of stressing the sense of family and unity from orientation forward. The facility should instill a sense of common purpose in employees to the point where they start holding each other accountable.
-
A defined performance improvement approach that goes beyond service recovery. Service recovery can add to patients' perceptions, but the organization must take proactive measures to identify and address ongoing problems, particularly those that extend beyond the unit level. Healthcare systems often create so many special teams and committees that each group's responsibilities and role are not clear. The best performance improvement teams have a defined mandate or charter and clear communication channels, and they provide constant communication on their progress to others.
-
A proficiency in baseline tactics such as rounding, using whiteboards for pain management, and establishing "no pass zones." 优蜜传媒finds these efforts necessary but not sufficient for improving the patient experience. For example, rounding can be even more effective when the information is trended and used as a performance improvement tool. Hospitals also can take a more comprehensive approach to discharge planning. Facilities can focus on process or discharge materials, for example, without factoring in elements such as wait time or the attention staff members pay to the patients between the time they are told they are discharged and the time they actually get to leave the hospital.
Senior leadership's responsibility
Improving the patient experience is about changing a hospital's culture, and this change is the single most powerful and legacy-defining step a leader can take to improve the care for a community. Senior leadership must not only take responsibility to make the patient experience a priority but also must allocate the necessary time and resources to make this focus a reality. Without this backing and accountability, any efforts to improve the patient experience will not succeed.
This article is adapted from one originally published in Middle East Health. Reprinted with permission.